FA16 Immunization Module’s Updates
Recent advances in vaccine technology: mRNA vaccines
The concept of messenger RNA (mRNA)-based vaccines has existed for around 30 years, but recent advancements in delivery have made mRNA vaccines an exciting area of development in vaccine technology. Just this month, Moderna Therapeutics received an award of up to $125 million to create a mRNA vaccine for Zika virus, and Genentech invested $310 million in a collaboration with BioNTech to develop individualized mRNA cancer vaccines.
Some unique advantages of mRNA vaccines are that they: 1) can be programed to encode any viral, bacterial, or parasitic proteins, 2) take a shorter amount of time to manufacture than traditional vaccines, 3) are not as risky as using inactivated viruses or pathogens, 4) are safer than DNA vaccines because they cannot mutate and integrate into the host genome, and 5) circumvent the complications of using adjuvants, which protein-based vaccines require. RNA vaccines do not need an adjuvant because they induce a stronger immune response by getting the host cell to translate many copies of the proteins they encode. They can also be used to vaccinate against cancer by training the immune system to recognize proteins that are known to be specifically produced by tumors.
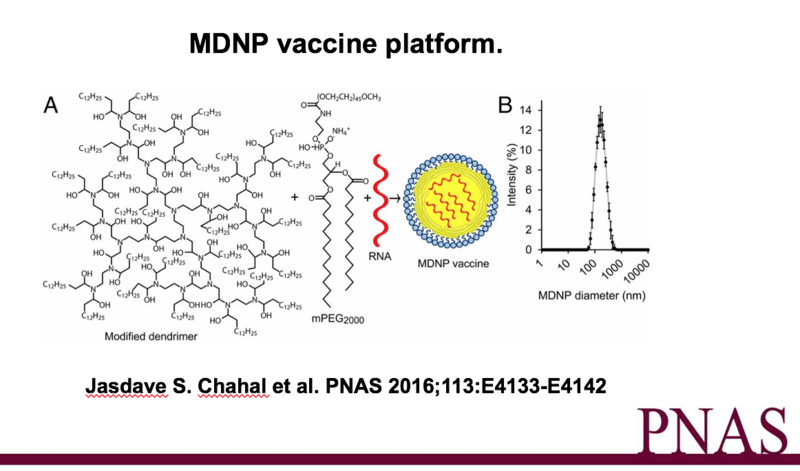
One particularly promising mRNA vaccine technology from a team at MIT and Harvard allows for immunization against multiple antigens (from the same or different microbes) in one injection. In this vaccine, RNA replicons (mRNA containing a start signal, code for protein, and a stop signal) with amplification instructions are packaged into nanoparticles made of molecules called dendrimers. These dendrimer nanoparticles can be made to be of a similar size as a virus, and thus are able to use the same surface proteins as viruses to enter cells.
In a recent paper published in the Proceedings of the National Academy of Sciences, the team demonstrated that this vaccine led to full CD8+ T-cell and specific antibody responses. In mice, a single dose of vaccines targeting Ebola, H1N1 influenza, or Toxoplasma gondii provided protection against exposure to lethal doses of the real pathogens. In addition to being “100% effective”, there were no adverse effects such as an inflammatory cytokine storm or signs of an immune response against the nanoparticles. The vaccine is easily administered through intramuscular injection, and can be designed and manufactured within a week. This is much more rapid than conventional vaccines which take around 6 months to produce. The team wants to create vaccines for Zika virus and Lyme disease as well, and this technology could be incredibly important for pandemics and outbreaks of flu and other viruses yet to be seen.
References:
Chahal JS, Khan OF, et al. (2016) Dendrimer-RNA nanoparticles generate protective immunity against lethal Ebola, H1N1 influenza, and Toxoplasma gondii challenges with a single dose. Proc Natl Acad Sci U S A 113(29):E4133-42. doi: 10.1073/pnas.1600299113.
Komaroff, AL (2016) Nanoparticle RNA Vaccines Are Remarkably Effective in Mice. NEJM Journal Watch (http://www.jwatch.org/na41904/2016/08/25/nanoparticle-rna-vaccines-are-remarkably-effective-mice)
Trafton, Anne (2016) Engineers design programmable RNA vaccines. MIT News (http://news.mit.edu/2016/programmable-rna-vaccines-0704)


Wow, thanks all for the insightful input and discussion. I am by no means an expert on any of this, but I can try to answer some of these questions based on my reading of the paper.
@Amanda Johnson That’s a great point. Hopefully these new vaccines technologies will indeed fewer side effects in humans as well, and help mitigate some of the stigma against vaccination.
@Steven Lee Based on the findings of this paper, yes, it should be possible to vaccinate against a wide range of strains of disease in one vaccine using this platform, as multiple replicons can be packaged into different nanoparticles and delivered at the same time (the authors of the paper call this “multiplexing”). One potential limitation is the length/size of RNA replicons being packaged into each nanoparticle, given that the effective nanoparticles are only ~150nm in diameter.
@Hannah Stein @Sara Sun @Jarod Shelton @ Christina Tsai Indeed, maintaining the stability of RNA has definitely been the greatest challenge in developing these vaccines. For this particular technology, it seems that the dendrimers indeed play a great role in stabilizing the RNA (they can be given a temporary positive charge and bind to negatively-charged RNA). In the paper, they used a variety of methods to demonstrate the stability of the nanoparticles and encapsulated RNA. In whole human serum, the nanoparticles remained intact and did not release the RNA payloads, which the authors suggest can protecting the RNA from degradation by endonucleases. This vaccine also uses mPEG2000 (methoxy polyethylene glycol), which is a commonly used coating for nanoparticle delivery systems because it has high biocompatibility and can be modified for specific delivery. For example, in many micelle and liposome-based systems using mPEG, peptides are conjugated to the surface of the nanoparticle to facilitate targeted delivery.
@Sara Sun I believe there are some other researchers developing mRNA-based vaccines for HIV! Many of the papers on these vaccines are from this past year as well, but I have not had a chance to read through them.
@Christina Tsai I agree, it would be super cool if CRISPR-Cas systems could be used for vaccines too someday.
Victoria this is an interesting advancement in the field of using RNA for medical purposes. I am curious how they will engineer the delivery of this, as it can degrade, just as Jarod and Dr. Tapping mentioned above. This concept also reminds me of how researchers have been able to use the CRISPR-Cas system to target RNA. This new technology certainly seems promising, especially with the spread of Zika virus.
Great post, real interesting topic! I had no prior knowledge about mRNA based vaccines. Its ability to protect against Ebola and other types of infections make it a promising tool for disease prevention. I remember the ebola outbreak a couple years ago and the frenzy it caused. A vaccine to protect against ebola would help put peoples minds at ease during another outbreak.
Very thorough! This is an exciting avenue of science and I cannot wait to see what becomes of this research! I believe that using mRNA based vaccines will become more common as the understanding of other RNA technologies improves. As I understand it, the delivery of any RNA-based therapeutic is relatively difficult due to degradation of the product following administration. The short half life of RNA drugs limits their ability to treat certain disorders, e.g. ASOs and ALS, however, providing a vessel for the RNA will most likely solve the issue. I will have to read the article to fully understand the concept, but you did an excellent job of summarizing the important concepts!
@Victoria Lu, This is a brilliant concept. So incredibly simple in a way that you can hijack the endogenous system to encourage its own immunity without risking adverse effects. As with many fascinating concepts, I am curious to see how this translates from the animal model to the human one. Although I realize this goes without saying, our bodies incredibly cunning; many concepts that otherwise seem successful in mice do not play out well in humans. Specificity and the stability of RNA certainly play a major role, although in the human organism, these limitations may be one of many. Thank you for your elaborate and eloquent post.
I think this advancement in the development of RNA vaccines is exciting! I'm impressed by the design of replicon delivery via dendrimers. @Hannah Stein brings up a good question about RNA stability--are the dendrimers designed to include some sort of RNA stabilization component? I also wonder if this technology is effective in individuals with retroviral infections. It will be intriguing to find out how the results transfer over from mice to humans. Thanks, @Victoria Lu, for this informative post!
@ Victoria Lu Not being overly familiar with the concept of mRNA vaccines nor their advantages, I found your update to be very informative. The success of the MIT and Harvard team is promising. As @Richard Tapping mentioned above, it will be interesting to see the effectiveness of such vaccines in clinical trials.
Cutting edge stuff. I love the key advantage of RNA- over DNA-based vaccines. RNA is generally highly susceptible to degradation, I don't know how they have overcome that hurdle. Definitely worth watching this technology as it moves into the clinic.
Victoria, thanks so much for picking such an interesting topic. I knew about the potential of RNA vaccinations for certain types of cancer. However, I never really thought about all the huge benefits of RNA vaccinations on a broader scale. Removing the risks associated with live attenuated and DNA vaccines would be huge. The only thing I wonder about is the stability since RNA is much less stable than DNA. Do you know if the studies are having any trouble maintaining the stability of the RNA vaccines or what they use to ensure that RNA vaccines are stable enough to store and transport?
This is a fascinating concept. It seems from your update that there is no current clinical trials being conducted, but could be in the near future. The use of RNA replicons, I believe, could also be useful in combating mutagenic pathogens. If I remember correctly, current flu vaccines target the surface cell receptors, which is why we have to take the flu vaccine every year. Could it possible to vaccinate against a wide range of different strains (different cell receptors) of the flu or another disease? This could allow for individuals to be vaccinated against diseases which are normally troublesome to vaccinate against.