FA16 Immunization Module’s Updates
Vaccine for Treatment of Prostate Cancer
Prostate cancer is the most commonly diagnosed cancer and is the second leading cause of cancer-related death for men in the United States.
Cancer vaccines stimulate or restore the immune system’s ability to fight infection and disease. While most vaccines help prevent infections, a vaccine has been developed that boosts the immune system to actively attack prostate cancer cells. Sipuleucel-T (Provenge) is the only FDA-approved cancer treatment vaccine. Prostate cancer lends itself well to this approach because the target proteins are expressed almost exclusively in prostate tissue, making effects on other tissues unlikely.
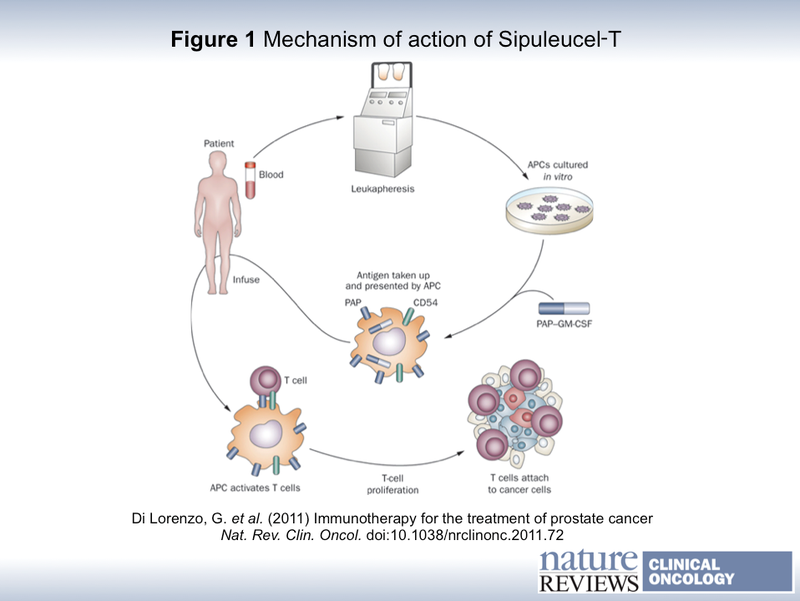
The vaccine is made specifically for each patient. In order to sensitize the immune system to tumor cells, a patient’s peripheral APCs are isolated, exposed to the tumor-associated antigen prostatic acid phosphatase (PAP), and reinfused 72 hours later (see image below). The APCs will ultimately cause production of antibodies and activate cytotoxic T cells to kill cancer cells.
A phase 3 trial showed that patients receiving Sipuleucel-T had a greater median overall survival rate compared to those receiving placebo (25.8 months to 21.7 months). Sadly, it was used as a last resort in advanced prostate cancer and even this 4 month extension was considered a success. Currently, new vaccines are being developed that target multiple TAAs. Another budding area of research involves DNA vaccines, which can elicit antigen-specific T cells using a simpler platform. Advances in technology are changing the way we think about treating cancer, utilizing our immune system rather than attacking cancer cells directly.
1. Lorenzo, Giuseppe et al. “Immunotherapy for the Treatment of Prostate Cancer.” Nature Reviews Clinical Oncology 8 (2011): 551-61
2. Rekoske, Brian T and Douglas G Mcneel. “Immunotherapy for Prostate Cancer: False Promises or True Hope?” Cancer (2016)
3. http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-treating-vaccine-treatment
4. https://www.cancer.gov/about-cancer/causes-prevention/vaccines-fact-sheet#q4


@Jarod Shelton: Good point: I forgot PSA is secreted, so its surface MHC presentation is going to be a bit more limited. There should be a lot of unusual antigens available to target, given the crazy abnormal expression patterns seen in metastatic cancer. I suppose we just have to find them, which can take some time.
This opens up a whole new avenue of cancer treatment. I performed a brief search and a number of additional studies have been conducted to examine the efficacy of Sipuleucel-T (Provenge). The studies I reviewed, Barar and Omidi (2015; PMID: 26191499) and Messerscmidt et al. (2016; PMID: 26834161) report that their is statistical significance in the increased survival rate of patients treated with Provenge. Hopefully researchers will be able to streamline the procedure to make the therapeutic widely available!
@ Tejasvi Niranjan. It may be difficult to develop a vaccine using PSA. PSA is a secreted protein that would not result in the targeting and destruction via APC. Maybe an antigen could be targeted on the epithelial cells that are responsible for the increased PSA secretion? Let me know what you think!
It is interesting that they target Prostatic Acid Phosphatase, which can occur in increased amounts not only in prostate cancer, but has been largely been displaced as a marker for prostate cancer by PSA (prostate-specific antigen). I would hope that there is a pipeline to try the same immunotherapy system, but using PSA, as they could conceivably work for a broader set of prostate cancer stages.
@Matthew Law: Delivering antigen directly ex vivo to APCs likely circumvents one issue with DNA vaccines, which is that they may incorporate into the endogenous genome of the APC and have an oncogenic effect (though this has not be completely proven). It would be terrible to treat a patient's cancer only to induce another one: however, so many current cancer treatments are also carcinogens, so maybe from a clinical perspective it can be dealt with.
@Gabriel Swords @Sara Sun You bring up some good points! I don't know why this hasn't been tested on earlier stages of disease. My guess is that there are more traditional therapies (chemo/radiation) that may carry a greater chance of survival and patients/doctors are hesitant to risk a new therapy. Also, as you mentioned this individualized therapy would be expensive! As for the personalization of APCs, my guess is that either the antigen would degrade if introduced directly to the body, or would take a long time for an APC to find and present. Also, the free antigen might be harmful to the body. As mentioned in a different post, gene gun technology is being used to fire DNA or RNA directly into our cells in vivo to present the desired antigen, so that sounds like a promising area of research for all types of cancer. The challenge is finding an antigen that will target cancer cells without initiating an autoimmune response.
This is quite a fascinating read. Hopefully with more research that goes into this field can potentially lead to other approved vaccines that are specialized to target other types of cancers. Considering the prevalence of cancer, perhaps later on we'll see more novel immunotherapies.
Thanks, @Matthew Law, for the interesting update! This sounds like an important advancement in therapy to keep an eye on! As @Gabriel Swords mentioned, why has this not been tested more aggressively on individuals with earlier stages of prostate cancer, when there may reasonably be a greater effect on life expectancy?
I am also wondering how rapid is the cytotoxic T cell response with this method and why the personalization of APCs for this therapy is necessitated when it appears that the single antigen PAP is being targeted. Personalized medicine today is not yet affordable for or readily available to most patients. Is there a way this therapy could be designed as direct delivery of PAP antigen conjugated to some foreign component? And could this be extended even further and developed into a preventative vaccine against prostate cancer?
@Matthew Law, I find it very interesting that this vaccine is developed specifically for the patient. I think this highlights how one day we will be able to better individualize treatment for patients. Additionally is shows the importance of understanding what kinds of receptors on cells are expressed normally and in the diseased state. Using this information will lead to better treatments.
@Matthew Law A great example of the use of vaccines in cancer immunotherapy. This is a very exciting area that is beginning to show a lot of clinical promise!
I really like this method of treatment because it utilizes the body's natural defenses to help fight prostate cancer. I found it peculiar that this technique is only used as a last ditch effort in the later stages of prostate cancer. Have there been any instances where it has been tested in an earlier stage of the disease? Furthermore, are there any other potential applications of this technique besides prostate cancer?
Thanks for sharing!