New Learning’s Updates
Considering the Future of Medical Education
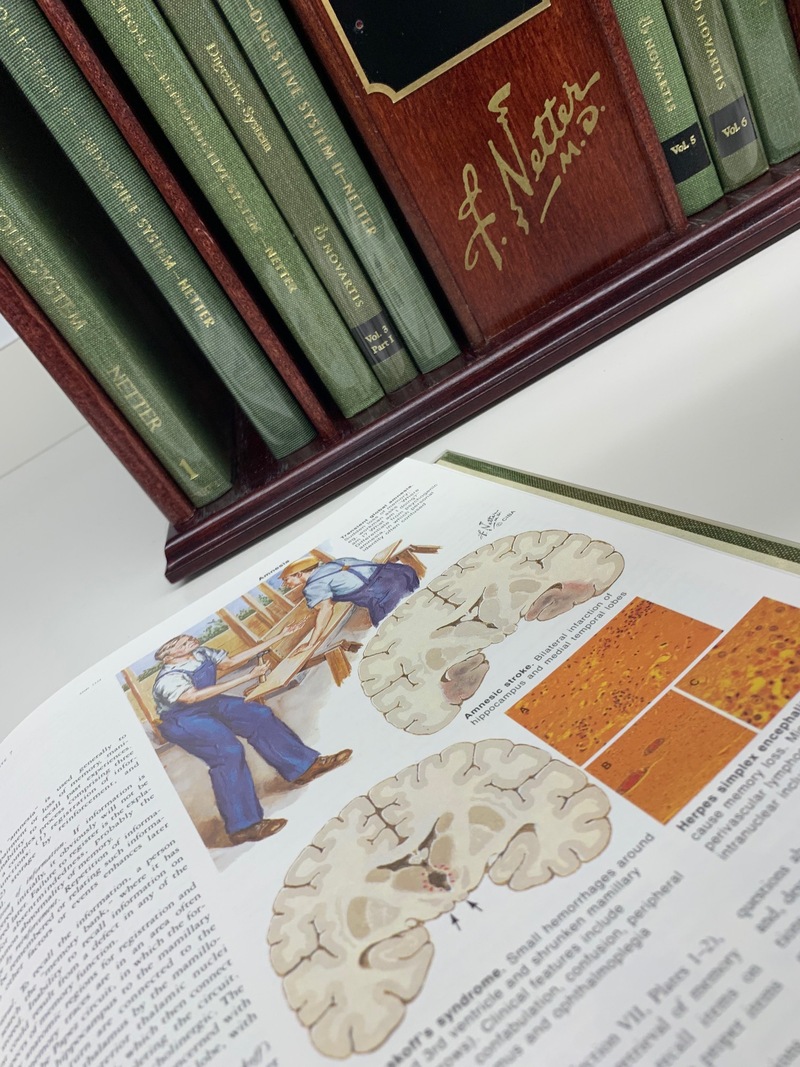
Mary Kalantzis and Bill Cope visited the University of Illinois College of Medicine in Peoria this week, on the invitation of NSF project partner, Dr Richard Tapping. The purpose of the visit was to explore shared teaching and reseach interests in the rapidly changing field of medical education.
In their NSF funded project, “Assessing Complex Epistemic Performance in Online Learning Environments,” Kalantzis, Cope, Tapping and their research colleagues have been investigating the development of critical clinical thinking in e-learning environments. Using the peer review function in the collaborative learning platform, CGScholar, medical students in the research study developed clinical case analyses. For instance, in one cycle of intervention, students developed analyses of cases of autoimmunity including rheumatoid arthritis, diabetes mellitus, lupus, and multiple sclerosis. When they conducted their peer reviews, they analyzed a different condition, but against the same clincial analysis rubric. The development of student thinking is tracked in CGScholar by “big data” analytics which record numerous small datapoints as students progress towards learning objectives. These objectives center around critical thinking and professional judgment, and not just the straightforwardly "correct" answers about fact and procedure that are the focus of traditional assessments.
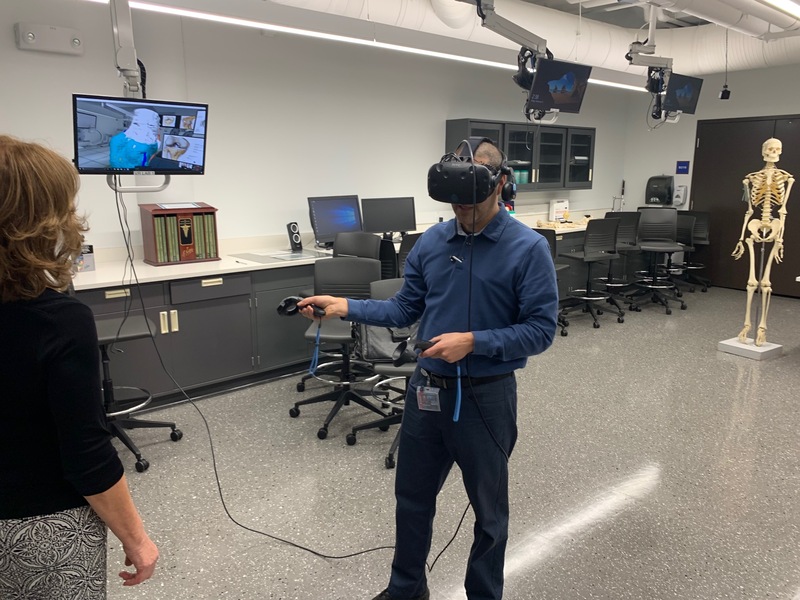
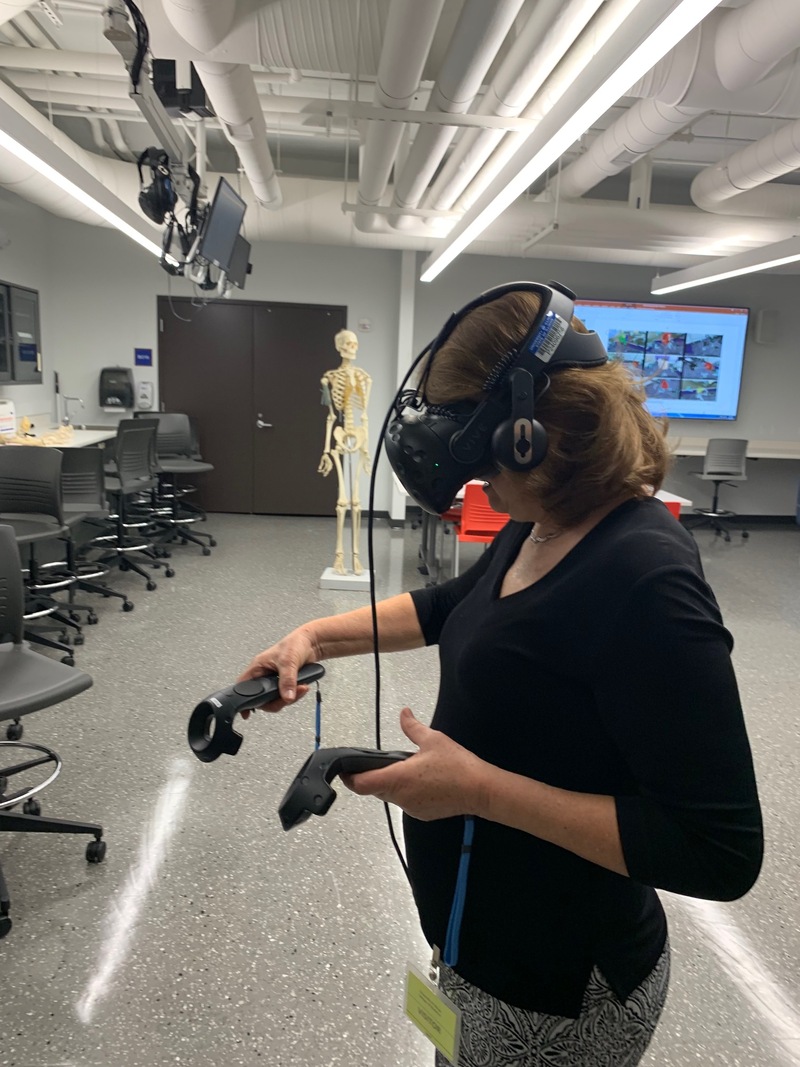
The visit to Peoria was an opportunity to share the outcomes of this research with other faculty, discuss directions in technology-mediated learning, as well as to explore opportunities for wider implementation and further research. It was also a chance to visit the world-leading Jump Simulation Center and to experience Enduvo, the cutting edge virtual reality teaching and learning program developed by faculty in the College of Medicine.




@Richard this sounds great. I like the multi-modal learning aspect. This really can be a great way to apply all the skills we are looking for.
Thanks
@Sol Roberts-Lieb,From my standpoint the advantage is less hindered peer-peer interactions. In this asynchronous environment the students have time to think and reflect before commenting. With the right rubric (for example presenting a clinical problem), the software is well suited to exercise the problem solving and clinical reasoning skills of students. Obviously however, it cannot replace real patient interaction which is far more complex since it involves asking the right questions and picking up on real time social clues. This is where simulated patient exercises (or something similar) may be needed to fill the gap.
@Richard thanks so much. I appreciate that information. I was curious as to the replacement of an in-person activity to this. I will read the paper more thoroughly to look at the satisfaction data. I'm very curious as to the balance between these type of activities and the clinical reason in patient interaction. Very interesting. I'm also looking to see if this is something we can/might implement here at Carle Illinois.
@Sol Roberts-Lieb In answer to your question, the autoimmunity project in Scholar replaced a previous TBL exercise on the topic. Scholar analytics were used to determine the student grades. We did collect student satisfaction data, some of this is provided in the paper referenced by Bill above (see pdf link). I felt Scholar did a great job promoting peer-peer communication and feedback (more than any live exercise where many students are intimidated to orally participate). I hope this helps. Best, Richard.
@Thedora Olufunke Bello, thanks for that comment! Actually, we're not making an in-person vs online distinction. For instance, on-campus students may be working in simulations, in-the-field students might be working with patients. The focus is critical clinical thinking using e-learning tools, whether online or not - at this level, the challenge is the same.
Dear Dr. Cope and Kalantzis,
Let me congratulate you for a job well done. The only issue i have with this your research is that, the students interactions were mainly online which was devoid of real life situations. In many cases, real life situations, psychological state of patients and other intervening variables which one could not control may serve as limitation and if same is carried out in real life situations might not result in the same outcome.
thank you
Theodora Bello
@Bill I couldn't agree more. We tell our students that the wrote facts can be looked up. How to think, how to solve problems, and the interconnectivity of everything is what we are trying to teach them. Some get it, others just want the facts to spit them back for the boards and figure they will learn the important stuff later. It's definitely a challenge but one that studies like this will help.
William Cope
@Sol Roberts-Lieb, the problem is that the students have got to where they are because they are good at exams, a kind of game, memorize a pile of stuff => get the right answers. When they resist because what we expect seems more or harder work, we say that being a medical professional involves collaboration; it involves judgement when the answers are not always clear; and that canonical medical knowledge involves peer review. These higher order forms of disciplinary thinking and professional practices are what we want them to learn. In this day and age, with look-up and data manipulation devices on our persons, we can leave lower level capacities and long term memory and to these cognitive prostheses (and in fact, they have can look up more than it would ever be humanly possible to remember), but humans still have to do the higher order stuff - this is what they are learning.
Thanks @Bill, I appreciate it. Agreed, old LMSes are basically file sharing with some collaboration tools added on, instead of a collaboration tools with file sharing available.
My wonder is tools are great, but does it really create new learning models for students, in this case, medical students.
What I have seen is while my students say they want active learning and new learning models, many just want a direct lecture to try to inhale the content as it's easier than active learning. The fact that they retain the knowledge better when integrated with hands in clinical experience or activities, is second to can they comprehend the knowledge to pass board exams.
Of course, I hope the board exams change soon, but I don't know as residency programs want an objective way to narrow down applicants.
@Sol Roberts-Lieb, this was an experimental intervention, so no, it did not replace current learning management systems or assessments. But the purpose of our research is to consider what a next generation of learning management system would look like. The reality of all major learning management systems is that they are based on 25 year old file sharing technologies. We're experimenting with new models, with systematic peer interaction, big data analytics, and just-in-time formative assessment. So the bigger picture question for us, is what are the pedagogical possibilities?